AI Program to Teach Physicians How to Have End-of-Life Discussions
by Henry Fersko-Weiss
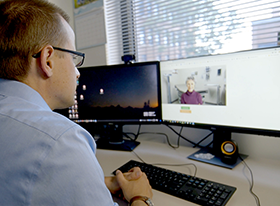
It is no secret that many physicians struggle with end-of-life discussions with their patients. Researchers working on ways to improve physician-patient interactions around difficult conversations have employed actors to role-play patients, but the timing and cost required poses a challenge to employing that tactic more widely. To address the need for an approach physicians can easily and comfortably use, researchers at the University of Rochester have developed an artificial intelligence (AI) system utilizing a computer-generated avatar as a patient. The program is in its final stages of development and testing. When released it will allow doctors to practice these delicate end-of-life conversations and give them immediate feedback and areas for improvement.
University of Rochester
The program, called SOPHIE, which stands for Standardized Online Patient Healthcare Interaction Education, appears as an on-screen human face and upper body. This avatar of a patient starts the conversation by stating some facts and raising questions. Palliative care expert Ronald Epstein and his team at the Rochester University Medical Center analyzed over 400 conversations between oncologists and late-stage cancer patients, which became the source for SOPHIE’s responses and questions. Next, researchers from the Rochester Human-Computer Interaction Lab, under the supervision of Ehsan Hoque, applied algorithms to the conversations to program SOPHIE and to develop a series of metrics that assess how well a physician communicates end-of-life concerns and care options.
According to an article in the Rochester University Newscenter publication, 68% of late-stage cancer patients leave their doctors’ offices without fully understanding the severity of their illness, overestimating their life expectancy, or both. To help physicians do better, a conversation with SOPHIE begins with the avatar stating that she has lung cancer and asking about her nightly sleep pattern and the need to adjust her pain medication. Then SOPHIE asks about her test results and prognosis, expresses some of her fears and concerns, and asks if chemotherapy is still an option or whether she should shift to a focus on comfort care. At the end of the conversation, SOPHIE asks how to break the news to her family.
The system collects data on physician responses throughout the interaction. At the end of the conversation, physicians can see a graphic that shows how many questions they asked, how many of those questions were open-ended, and how much time they spent lecturing the patient without giving ample time for responses and queries. The system also displays a chart of the “sentiment trajectory,” which reflects the use of positive words and phrases to increase patient understanding. Doctors who tested the system report that the conversation with SOPHIE feels very natural.
Next, SOPHIE will be put through a randomized, controlled experiment to demonstrate its effectiveness before first-year students at the Rochester Medical Center begin to use the system. Ultimately SOPHIE will be available through a computer browser, accessible to physicians anywhere for practicing end-of-life conversations and improving their skills in conducting them.
