News Briefs – JULY-AUGUST 2021
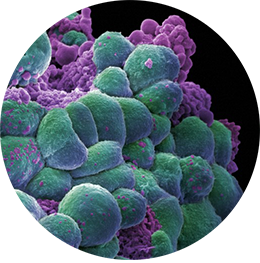
Annie Cavanagh/Wellcome Images
A Promising New Approach Kills Breast Cancer in Mice
A research team led by scientists at the University of Illinois Urbana-Champaign recently reported the development of a drug called ErSO in Science Translational Medicine. ErSO quickly kills 95-100% of breast cancer cells in mouse models of human estrogen receptor–positive breast cancers—the most common form of breast cancer—and their metastases in bone, brain, liver, and lungs. It is currently incurable in its metastatic form. ErSO quickly shrinks even large tumors to undetectable levels within a matter of days.
The new compound binds to the estrogen receptor and stimulates the overproduction of proteins that protect the cell by selectively killing breast cancer cells. ErSO has had no detectable side effects in the mice. One of the unique attributes of the drug is that it doesn’t affect healthy cells—even ones that have an estrogen receptor—but is potent against estrogen receptor–positive cancer cells.
ErSO is unlike tamoxifen and fulvestrant compounds, which are currently prescribed to block estrogen signaling in breast cancer. While ErSO binds to the same estrogen receptor, it targets a different site on the receptor and attacks a different cellular pathway.
Since about 75% of breast cancers are estrogen receptor–positive, ErSO represents the potential to cure the most common form of breast cancer. And it’s possible that ErSO would also work against some breast cancers not usually considered to be estrogen receptor–positive.
Further studies in mice showed that exposure to the drug had no effect on their reproductive development. It was also very well tolerated at much higher doses than what is required to be effective. Many of the breast cancers shrank by more than 99% in just three days. The pharmaceutical company Bayer AG has licensed the new drug and will explore its potential for further study in human clinical trials. Researchers will next study the effectiveness of ErSO against other types of cancers that contain an estrogen receptor.
Knowledge of Palliative Care in the U.S. Is Extremely Low
A recent analysis of 2018 data from the National Cancer Institute published by the American Association of Cancer Research revealed that only about 11% of people in a survey of 3,450 respondents had adequate knowledge of palliative care. Compounding this problem is the fact that physicians tend to make a palliative referral late in the patient journey, even though palliative care has been proven to improve the quality of life for patients and caregivers by addressing the physical, psychological, and emotional challenges associated with cancer and its treatment. Palliative care has also been associated with increased patient satisfaction.
The survey asked respondents how they would describe their knowledge of palliative care. Possible responses were: “I’ve never heard of it,” “I know a little bit about palliative care,” and “I know what palliative care is and could explain it to someone else.” When the results from the first two responses were grouped together, they showed that about 89% of respondents had inadequate knowledge of palliative care. Women and married couples were twice as likely as men and singles to have competent knowledge. Other respondents with a higher understanding of palliative care were people with a university degree, those who utilized the health care system frequently, and people previously diagnosed with cancer.
Health care providers are often the first source of medical information for patients, so educating physicians about palliative care and encouraging them to discuss it with patients and caregivers could lead to greater utilization. Other barriers the survey identified are a misunderstanding of palliative care, lack of resources to provide that care, and inadequate time for discussions with patients.
One limitation of the survey is its self-report methodology. However, the survey researchers point out that how people perceive their knowledge of palliative care can affect their confidence and how likely they are to ask for it.

HQuality/Shutterstock
Spending Time Outdoors Is Good for the Brain
During the COVID-19 pandemic, many people discovered the mood-boosting effect of spending time outdoors. Simple acts such as strolling in a park, hiking in the woods, and sitting on the beach do more than just provide relief from being indoors—they improve people’s general sense of well-being. A recent study suggests an even more profound impact of time spent outside: It alters the structure of the brain for the better.
The study, conducted by the Max Planck Institute for Human Development and the University Medical Center Hamburg-Eppendorf, indicates that being outside can be linked to higher gray matter volume in a part of the brain’s prefrontal cortex. In addition to improving mood, this structural effect on the brain is likely to have a positive impact on concentration, working memory, and overall psychological health.
The researchers regularly examined six healthy, middle-aged individuals over a period of six months. More than 280 MRI scans of their brains were conducted during that time. The study looked at self-reported behavior during the previous 24 hours, particularly the hours they spent outdoors prior to a brain scan. There was a direct correlation between time outdoors and gray matter volume, even when other factors—such as fluid intake, consumption of caffeine, and physical activity—were taken into account.
Oncologists Frequently Miss Opportunities for End-of-Life Discussions
A study recently published in JAMA Network Open found that oncologists regularly miss opportunities for end-of-life care discussions with their patients. This is concerning because it indicates that decades of efforts to improve oncologist communication have had little impact on behavior. The result for patients is that aggressive, burdensome, and expensive end-of-life treatments continue when the right conversation might have led to a gentler dying experience.
The authors of the study defined a missed opportunity as one in which the oncologist failed to explore a patient’s values, goals, or preferences despite a clear opening in the conversation where such a discussion would have been appropriate, even necessary. Topics oncologists could have discussed with advanced cancer patients included discontinuation of treatment, advance care planning, palliative and hospice care, as well as after-death wishes. The authors noted three ways oncologists tended to deflect patient discussions relating to end of life: inadequate response to concerns about disease progression, the use of optimistic future talk, and expression of concern over discontinuing treatment.
The investigators analyzed five years of audio recordings of outpatient visits that were conducted for the Studying Communication in Oncologist-Patient Encounters randomized clinical trial. In total, the study included 423 visits with 141 patients in two academic medical centers. Only 5% of visits included discussions on end-of-life topics or choices.
The authors concluded that future efforts to improve oncologist communication around these difficult subjects would require addressing fear of upsetting patients, discomfort engaging in end-of-life discussions, the challenges of providing a better prognosis, and responding to patient emotions with empathy.
