News Briefs – JUNE 2021
MDMA Eases Symptoms of Severe PTSD
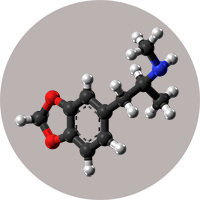 A new clinical study utilizing MDMA, a psychoactive drug, along with short-term intensive therapy has shown very promising results in alleviating the symptoms of severe Post Traumatic Stress Disorder (PTSD) for people who have suffered for years. This is further evidence that psychedelics like MDMA, psilocybin, Ketamine, and others have a place in the treatment of depression, addiction, and fear of dying in people with a terminal illness.
A new clinical study utilizing MDMA, a psychoactive drug, along with short-term intensive therapy has shown very promising results in alleviating the symptoms of severe Post Traumatic Stress Disorder (PTSD) for people who have suffered for years. This is further evidence that psychedelics like MDMA, psilocybin, Ketamine, and others have a place in the treatment of depression, addiction, and fear of dying in people with a terminal illness.
According to Make the Connection, an online resource for veterans, 7-8% of U.S. adults suffer from PTSD each year. That percentage rises to 11- 20% for veterans, depending on the war or operations they participated in. More than a third of people with PTSD suffer with severe symptoms.
The results of the study, published in Nature Medicine last month showed that 67% of the participants who took the MDMA had improved so markedly after the 18-week trial that they no longer met the diagnostic criteria for PTSD when evaluated by independent clinicians. Since PTSD is often a lifetime struggle and can surface as a major difficulty when facing end of life, this substantially positive result gives cause for great optimism that an effective treatment is getting closer. However, further studies are necessary, which is made more difficult because MDMA remains a prohibited drug in the U.S.
Medical Aid in Dying Updates
Here are some of the latest news items in the effort to advance Medical Aid in Dying (MAID) in the U.S.:
- According to a report in NJ.com, 33 terminally ill people chose to use New Jersey’s MAID act last year, joining the 12 people who made that decision in the last five months of 2019, the year the act became law. Nearly 90% of the individuals chose to die in their own home. Of the 33 people: 24 had cancer, 5 had ALS, 2 had pulmonary disease, and 2 had either a stroke or cardiovascular disease.
- A bi-partisan bill was introduced in the Pennsylvania legislature to allow terminally ill patients to request end-of-life medication from their doctor. The bill, which was referred to the state’s House Judiciary Committee, will require a physician to inform a patient about alternatives, such as hospice and pain management. Patients will also be encouraged, but not required to inform their close relatives about their decision.
- The California legislature is studying ways to remove roadblocks to its five-year old End-of-Life Option Act. One of the changes would make it harder for physicians to refuse to participate. Another would delete a clause in the act that allows it to expire in 2026. The bill has been passed by a state Senate committee.
Using Virtual Reality to Teach Caregivers Empathy

Alamy
Over the past 20 years there has been a growing interest in using virtual reality (VR) as a teaching tool. Last month in the Journal of Medical Imaging and Radiation Sciences a group of researchers published a review of 7 studies involving 485 caregivers to teach people empathy through VR. All seven studies demonstrated that VR could elicit empathetic behavior, suggesting that it might be a useful tool for teaching empathy. Unfortunately, none of the studies assessed the long-term effects of VR on acting empathetically.
One of the findings from this study was that simulated experiences where the person takes on the role of the individual receiving care appear to be the most effective. But the authors recommend that future studies need to incorporate a multicenter, randomized and controlled design to figure out which VR experiences are the most effective in evoking empathetic behaviors.
Empathy is essential to patient-centered care for clinicians, technicians, end-of-life doulas and family or friends who take on the caregiver role. Empathy has been shown to provide appropriate support, increase patient satisfaction, enhance patient outcomes, lead to fewer mistakes, and offer better overall care.
The authors talk about two forms of empathy: affective and cognitive. High levels of affective empathy, in other words a strong connection to another person’s emotions, has been associated with increased levels of stress, compassion fatigue, and decreased quality of life for caregivers. On the other hand, cognitive empathy, the ability to deeply understand another’s emotions, leads to improved care provision and the wellbeing of the caregiver. This analysis supports how important it is for doulas to maintain affective boundaries with the people they serve.
Advance Care Planning Allows Patients to Achieve 90% of their End-of-Life Wishes
According to recent research published in the Journal of American Medical Association Network Open, people who inform their loved ones and health care providers about their end-of-life care wishes find that 90% of the time those wishes are carried out. This research was conducted among 715 Kaiser Permanente families in which a person 65 or older had died.
Not only did 89% of those families report that their loved one’s wishes had been met, but they also reported that 94% had not received unwanted treatment. Yet in a 2017 study published in the Journal of the American Geriatric Society only 14% of individuals with a serious illness had an advance care plan (ACP) in their electronic health records. That same study showed that of the patients receiving palliative care, 65% had an ACP, while only 11% of those not having palliative care had an ACP.
Difficulty in talking about end of life appears to be part of the reason for people failing to create an ACP. A 2018 report from MacMillan Cancer Support in the UK speaks to this. It revealed that only 35% of people who said they had thoughts and feelings about their death had shared those feelings with anyone. And, only 8% of those people had spoken to their healthcare providers about the subject.
