News Briefs – MAY 2021
The Proportion of Black Physicians in the U.S. has Grown Little in 120 Years
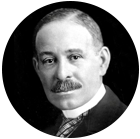
Dr. Daniel Hale Williams founded the first black-owned and non-segregated hospital in America, and performed the world’s first successful heart surgery, in 1893. agefotostock/Alamy Stock Photo
A new study conducted at the University of California, Los Angeles (UCLA) analyzing U.S. Census data from 1900 to 2018 shows that the proportion of Black physicians has grown very little over nearly 120 years and remains far lower than the proportion of Black people in the nation’s population. As of 2018 only 5.4% of physicians were Black, even though 12.4% of Americans are Black.
Since 1940 all of the growth in Black physicians has come from women entering the profession. The number of Black men who are doctors has actually shrunk slightly over the past 80 years.
The study also showed the median income for Black male physicians was significantly lower than their White counterparts. This study reveals how much work still remains to make the medical profession more inclusive. Read more details at the Journal of General Internal Medicine.
Anesthesia as an Option in End-of-Life Care
In the United Kingdom and other parts of Europe where medical aid in dying is illegal, anesthesia is being considered as an alternative for people whose distress or pain can’t be well managed at end-of-life. This approach may also be used for people close to death who clearly express a wish to be “asleep” as they die.
According to an April 27 article in The Conversation, a network of not-for-profit media outlets that publish news items written by academics, this use of anesthesia ensures that the dying person is completely unconscious without hastening death. The authors had surveyed more than 500 people in the U.K. last year about end-of-life options. Nearly 90% said they would like to have the option of anesthesia if they were dying.
In another April article in the publication Anaesthesia, published by the U.K. Association of Anaesthetists, the authors from Oxford University explored the medical, procedural, ethical, and legal issues of this expanded use of anesthesia beyond its surgical applications. Although the data is currently limited, the article states that using the anesthetic Propofol in gradual titration to induce unconsciousness has been successfully maintained for up to 14 days without suppressing spontaneous breathing. The conclusion of the authors is that “There is a strong ethical case for making this option more widely available.”
Here in the U.S., outside of the 9 states and Washington D.C. that have some form of medical aid in dying, the only alternatives for alleviating intractable suffering at end of life has been voluntarily stopping eating and drinking (VSED), which itself can cause great discomfort, or palliative sedation. Palliative sedation, as the name implies, has relied on utilizing sedatives, barbiturates, neuroleptics, hypnotics, and other similar medications. This approach has had a contentious history because of confusing definitions and disparities in clinical use. Thus, it has rarely been used.
Anesthesia at end-of-life would give dying people a new way to alleviate suffering without accelerating the dying process. One drawback to this approach is the need to have an anesthesiologist involved in administering and monitoring the dosing. More information can be found at The Conversation and Anaesthesia.
Efforts to Reduce the Misuse of Opioids May be Hindering End-of-Life Pain Management
The Oregon State University College of Pharmacy in April reported there has been a decreasing trend in opioid prescriptions for dying patients based upon data from more than 2,500 hospice patients over a nine-year period. This could indicate that some patients may have been undertreated for their pain.
Five years ago, in response to the national epidemic of overprescribing opioids, the Centers for Disease Control and Prevention (CDC) issued guidelines to curb opioid use. However, the intention wasn’t to reduce the appropriate use of opioids for patients at the end of life, according to Jon Furuno, the lead author and an Associate Professor and Interim Chair of the Oregon State Department of Pharmacy. He noted that more than 60% of terminal cancer patients report very distressing pain. He went on to say, “Our results quantify a decrease in opioids among patients who are often in pain and for whom the main goal is comfort and quality of life.”
The article reported a decrease in opioid use on the first day of hospice care for patients who had been discharged from the hospital and had received an opioid prescription within the last 24 hours of their hospital stay. Furuno noted that “…interruptions in the continuity of pain treatment on transition to hospice are associated with poor patient outcomes.” For more information read the full report here.
Hospices Need to Better Serve Patients with Disabilities

wavebreakmedia/Shutterstock
Patients with disabilities have been largely underserved by hospice in spite of the fact that almost 40% of people aged 65 or older have at least one disability, according to a 2014 Census Bureau report. And, an April article in Hospice News states that the number of seniors older than 65 who have an intellectual or developmental disability is projected to double by 2030.
Mobility issues as well as difficulties with hearing, vision, and cognition result in limited ability to perform tasks of daily living, such as bathing, dressing, and eating. Only a small number of hospices across the country have programs specifically focused on patients who struggle with these core care needs.
ViaQuest, a hospice, home health care agency, and provider of behavioral and mental health care that operates in Ohio and two other states, has a Hospice Specialty Program for Individuals with Developmental Disabilities. This program provides medical, skilled nursing, and behavioral health services that specifically target the unique needs of patients with disabilities. According to Rick Johnson, President and CEO of ViaQuest, it’s the combination of the medical and behavioral approaches to care of people with disabilities that gives hospice clinicians the ability to provide quality end-of-life care.
Reaching more patients with disabilities will require that hospices invest in research, education, and staff training. To acquire the expertise they need, some hospices, like ViaQuest, are partnering with community organizations that offer specialized services. For further information read here
Advances in Smell Tests Could Provide Early Diagnosis of Parkinson’s Disease
Researchers at Queen Mary University of London developed an inexpensive, rapid, and easy to use smell test kit that has the potential to diagnose Parkinson’s disease. More than 90% of Parkinson’s patients suffer from loss of smell. Previous studies indicate that the right smell test could identify those at a high risk of developing the disease at least 10 years prior to more common symptoms.
To take the new smell test a capsule of aromatic oils is crushed between the fingers. The ability to recognize the smells generates a score which can be read immediately in a primary physician’s office. Previous smell tests involved a scratch and sniff approach that depended on the person’s capacity to scratch a paperboard hard enough to release enough odor to act as a reliable indicator of poor ability to smell. Those tests are not widely available, expensive, and take too long to administer in routine healthcare settings.
The amount of odor released in the new test is controlled by the amount of oil that is precisely encapsulated and placed between two strips of single-sided tape. The study of this test appeared in the April Journal of the Royal Society Interface. Lead researcher, Dr. Ahmed Ismail, stated the new test is more reliable and can be inexpensively mass produced. Misdiagnosis and living with uncertainty can be very stressful and frustrating for individuals who may be developing the disease.
